Pandemic policies inevitably require us to make decisions about whom to prioritize when it comes not only to saving lives, but also to promoting health, wellbeing, and life expectancy. When we talk about lives in this context, we are not only talking about whose lives to save. We are also talking about the quality that such lives will have as a consequence of our decisions, the physical and mental health outcomes of such lives, and whether to “save” lives in the short term or lives in long term, considering for example that the level of unemployment in young generations caused by restrictive measures will likely negatively impact their life expectancy. (I would ask those who are troubled by the term ‘caused’ here to wait until I address the point below).
One of the many slogans that has been used to try to accommodate facts to pre-formed narratives has been the idea that there actually is “no trade-off between health and wealth”, or that lockdown, while keeping infection rates down, also benefits the economy. So we should not attribute the economic crisis and unemployment rates to pandemic restrictions. Lockdown looks like a win-win. This is a nice narrative but, as this very precise analysis points out, it only works if lockdown manages to eradicate COVID-19 in the short term, as has happened in some countries such as New Zealand. For most high-income countries, that is not a realistic target and actually, in the long term, there is indeed a trade-off between the impact of lockdown in terms of economic costs – which will have a more significant impact on young generations’ prospects – and its impact in keeping infection rates low – which mainly benefits the elderly.
This wasn’t very well received, to say the least. Experts were quickly recruited by the press to rebut his claims. Headlines were made to convey people’s outrage at the idea that we can put a value on human life, and what is worse, different values on different human lives (which, by the way, is precisely what the NHS regularly does whenever it decides whom to put on a ventilator when there are not enough ventilators for everyone, or when it decides not provide life-saving treatments that cost more than £ 30k per quality-adjusted-life-year). 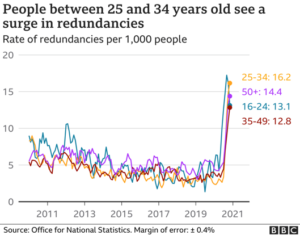
The benefits of lockdown mostly accrue to the elderly, who are significantly more vulnerable to COVID-19 with regard to risk of death and ‘long covid’, and significantly less impacted by restrictions.
“I don’t accept that all lives are of equal value. My children’s and my grandchildren’s life is worth much more than mine because they’ve got a lot more of it ahead. The whole concept of quality life years ahead is absolutely fundamental if one’s going to look at the value of these things.”
First, as the figures above suggest, the imbalance is at this point very significant and the cost on the worst off has grown very large. This does not necessarily make an imbalance unfair, but is a good indicator.
Former UK supreme court justice and historian Lord Jonathan Sumption recently made the following claim:
The fairest way of achieving the same goal ought to be preferred. This is very unlikely to be lockdown, because lockdown is ageist against the young.
Importantly, Lord Sumption’s claims make it explicit how a question about the trade-offs involved by lockdown is inevitably also a question around intergenerational justice. Here I suggest that current lockdown policies are an unfair form of age-based discrimination against young generations. That is, in philosophical jargon, lockdowns are ageist. “Ageism” is often assumed to be a form of unfair age-based discrimination toward the elderly. But current lockdowns are ageist against the young, or so I will suggest.
Oxford Uehiro Centre for Practical Ethics and Wellcome Centre for Ethics and Humanities
Thus, selective lockdown would not only be a fairer way of distributing harms and benefits of restrictive measures, but also a solution that would allow healthcare systems to cope with the pressure posed by COVID-19 by reducing infections in the groups more likely to be hospitalized.
The costs of lockdown are mostly on young generations, who are significantly less vulnerable to COVID-19 and significantly more affected by restrictions, both at present and in terms of medium and long term prospects. There are cases of “long covid” among the young, as there are cases of deaths. But these are rare and the most likely to experience lingering covid are the elderly and those with multiple serious medical conditions.
Thus, the young are disproportionately affected in terms of education opportunities, job prospects, and expected long term physical and mental health outcomes of lockdowns, and do not benefit significantly from the reduction of infections produced by lockdowns. The elderly benefit disproportionately by the reduction in infections produced by lockdowns because they are at higher risk of significant health consequences from COVID-19, including death, but will not be significantly affected by the implications of lockdown. They will not significantly suffer from unemployment and the long term socioeconomic impact of lockdown.
The question is whether this form of unequal distribution of costs and benefits across generations is unfair. There must be a threshold after which the sacrifices imposed on the young are simply too large and therefore this uneven distribution of benefits and harms across generations is unfair. There will inevitably be disagreement on where that threshold is and whether we are already past it, but that there is such a threshold at some point is really not disputable.
Second, a factor that makes imbalances or benefits and harms disproportionate or unfair is if the imbalance could be reduced at no significant cost. We should be prepared to pay some small cost to reduce imbalances for them to be fair and ethically justified. Accepting a certain imbalance when it could be reduced at some small cost makes the arrangement unfair. Evidence suggests that the actual benefit of lockdown-like measures compared to alternative forms of restrictions that do not involve stay-at-home orders and business closures is relative small and that “[s]imilar reductions in case growth may be achievable with less restrictive interventions”. It is unfair to simply accept this imbalance of harms and benefits when we haven’t taken this evidence into account and acted accordingly.
Third, imbalances of harms and benefits are unfair when there are reasonably available arrangements whereby those who enjoy the benefits would also take on more of the costs, compared to those who enjoy less benefits. An available arrangement to redistribute costs and benefits in a way that is more fair – that is, whereby those who get most of the benefits also take on more of the costs – while protecting public health systems is a form of selective lockdown, or shielding of the elderly and the vulnerable, as has been suggested early on in the pandemic but never seriously considered (see also the case for it in this document from October 2020).
Written by Alberto Giubilini
University of Oxford
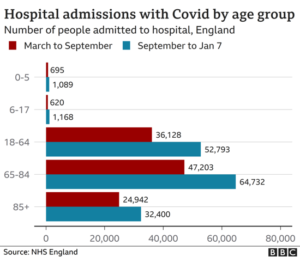
We also need to keep in mind that one of the main reasons, if not the main reason, in support of lockdown is the need to preserve public health systems’ capacity to take on new patients (both COVID-19 and non COVID-19). A system like the NHS is under unprecedented pressure and near capacity. While it is true that with the latest wave and the new COVID-19 variants hospitalisations increased across all age groups (including the young), it is still the case that, as reported by the BBC on 11 January, “the overall pattern of those at risk of becoming seriously ill or dying has not changed significantly”. As of 18 December 2020, hospital admission rates among the over 85s was almost 50 times higher than for those aged between 15 and 44 years, and the hospital admission rate was lowest among children aged between 5 and 14 years, at 0.6 per 100,000 people (ONS 2020). The table below shows the age distribution of hospitalizations in England in the period September 2020-January 2021, which covers the period of the spread of the new “English variant” of the virus. The 65-84 age range is quite large, but a selective lockdown that posed the threshold for shielding measures somewhere in that range, and very plausibly close to 80, would go a very long way in alleviating pressure on the healthcare system.
The last aspect is crucial because recessions, like the one we are having in the UK, are historically associated with higher morbidity and mortality and significant deterioration of mental health. This cost will be mostly paid by the young. To give just an idea, 1.72 million people in the UK are currently jobless (that is 5% unemployment), which is the highest figure in over 5 years, and those aged 25 to 34 have the highest risk of redundancies. The table below is pretty eloquent. This is in addition to the educational gaps of children because of school closure, increased levels of serious anxiety and depression during lockdowns reported by parents of school age children (who do belong to the young generations overburdened by restrictions and at low risk of COVID-19), and the exacerbation of various sorts of inequalities among young generations caused by education gaps. Keeping schools and universities closed contributes to these burdens and inequalities.
There are three reasons to think that we are already beyond that threshold and therefore that the imbalance of benefits and harms of lockdown mentioned so far is ageist against the young.
Sacrificing truth and rational reflection to fit pre-formed narratives has been a constant feature in this pandemic, which might partly explain why little progress has been made on seriously discussing options like those expressed in the Great Barrington Declaration about shielding vulnerable people while keeping society as open as possible, or making COVID-19 vaccination mandatory. For example, the current trend among academic and intellectual circles is to criticize the Swedish approach (Sweden never locked down and tried to strike a balance between restrictions and protecting the liberties and the economy) and to suggest that it failed miserably. But assuming facts still matter, Sweden has one of the lowest COVID-19 mortality rates in Europe and, very importantly, is one of the least affected economies when it comes to domestic gross product forecast.
If we want to ask the question and have a serious debate about this, we need to be prepared to accept uncomfortable answers, including the views that Lord Sumption’s has expressed. If we presuppose that such views are outrageously wrong and should not be expressed to begin with, we might as well avoid asking the questions and just go with common-sense narratives. Part of the outrage was due to the fact that a person with stage 4 bowel cancer was participating in the debate and felt (perhaps understandably) targeted by Lord Sumption’s claim. Cancer patients, even when young, are among the vulnerable people at higher risk from COVID-19. Because the kind of selective lockdown that Lord Sumption was defending would apply to all the vulnerable people, not just the elderly, she felt targeted by his remarks, although he clarified: “I didn’t say it was not valuable, I said it was less valuable”. Again, his claim needs to be read in the context in which it was made. But the context of the discussion matters. These claims were made during a TV program which posed the question whether current lockdown was “punishing too many for the greater good”. That certain lives might be less valuable than others, for the purpose of pandemic management, is built into the very same question that was being asked. Admittedly, “punishing” was a bad choice of words. “Harming” would probably have been better to refer to a series of restrictive pandemic measures, and most notably lockdown.
Reporting these figures, the BBC says that this is the grim situation “as Covid continued to hit the jobs market”. But this frequently used wording is misleading. These are more the result of pandemic measures, and most notably lockdowns, than of COVID-19 itself.
The elderly benefit more from restrictions because they are at higher risk from COVID-19. It is now well established that COVID-19 predominantly affects and kills old people, who are also way more likely than the young to be hospitalized. The best estimates place the COVID-19 infection/fatality rate (IFR) in high-income countries at 1,15%, but with a very uneven distribution across age groups. For the under 40s, the IFR is lower than 0.1%. Risk of dying doubles approximately every 8 years of age and raises to above 5% in the over 80s. As saw above, risks of ‘long covid’ are also much larger in the elderly and the vulnerable.

