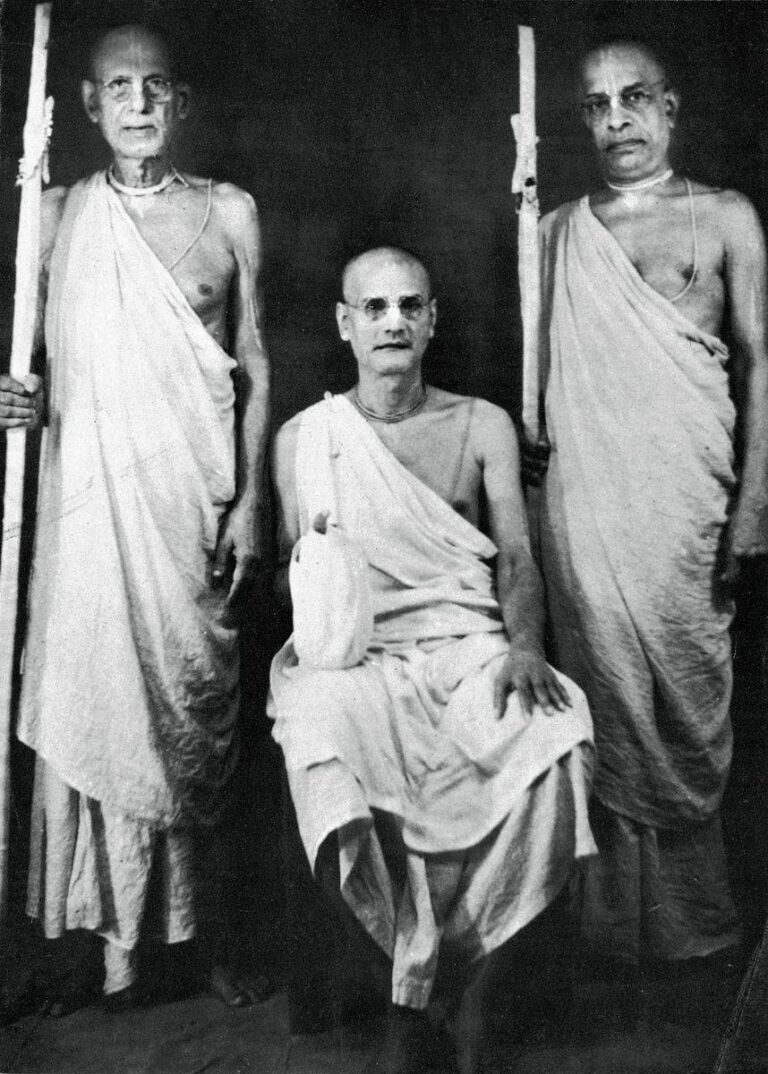
Prof Dominic Wilkinson & Dr Jonathan Pugh
“That is a tragic and distressing situation that we must do everything possible to avoid repeating.
First, we should ensure that all those who are high risk have access to vaccination. There are still approximately 10% of older adult care home residents who have not had a 2nd dose of the vaccine.
“It’s too soon to be talking about mandates. We’re still researching rare but potentially serious side-effects that have been thrown up by national monitoring, for example a possible link between Pfizer and myocarditis. We don’t have the full picture on how well they prevent transmission. Public Health England data about how transmission is only available for the first dose and it is currently at up to 50%. Meanwhile the level of protection afforded to vaccinated individuals themselves is holding up very well in terms of hospitalisation and death even against the new variants. With the level of confidence we have encouragement to vaccinate is warranted, and incentives are warranted. Mandates should only be made on the basis of bulletproof safety and efficacy data, including transmission data.”
Second, those who work in the frontline with vulnerable high risk patients have an ethical obligation to take all reasonable measures to prevent spread of the vaccine to those they are caring for. They must follow guidance about the use of measures like hand washing and PPE. They should take part in lateral flow testing schemes. And they should be vaccinated.
There is a strong ethical case that care home workers (and NHS staff) who have not had the COVID vaccine should be redeployed to areas other than frontline care.
It would be ethical to make COVID vaccination (in the absence of a medical exemption) a condition of employment in the same way that hepatitis B vaccination is currently for some health professionals.
Two (contrasting) perspectives on the news this morning about planned mandatory vaccination of care home workers.
If vaccines are made mandatory for health care and care home workers, they should be able to choose from available vaccines. Every effort possible should be made to address any concerns that they have about the vaccines.”
“In the earlier phase of the pandemic, some of the most medically vulnerable members of our community, patients in care homes and acutely ill patients in hospitals, ended up catching coronavirus from those caring for them. Some patients and care home residents died from infections that they caught from their caregivers.”
Professor Julian Savulescu
In England, as of 10th June, 17% of adult care home workers have not had the COVID-19 vaccine.
“The proposal to make vaccination mandatory for care home workers is muddle-headed. Vaccination should be mandatory for the residents, not the workers. It is the residents who stand to gain most from being vaccinated. Young care workers have little to gain personally from vaccination and there are now lethal risks, as well as uncertain long term consequences of novel vaccines. They have already risked their own lives during the pandemic. Some will be immune from past infection. Those remaining should be offered incentives, including financial incentives, to be vaccinated, not coerced. Vaccines like hepatitis and influenza may be mandatory, but they have been around for years and have established safety profiles.